
Expertise: Strategy, vision, team leadership, managing suppliers, design vision, digital strategy, content creation, editing, project management, innovation, child health, public health, modernising large institutions.
Location: London, UK 2001 to 2003
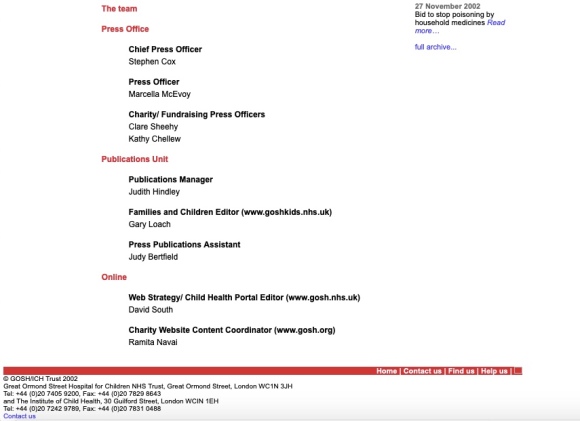
Project Manager: David South
Charity Content Coordinator: Ramita Navai
Click here to view images for this case study: CASE STUDY 5: GOSH/ICH Child Health Portal | 2001 – 2003 Images
Abstract
In 2001 I was hired to project manage and deliver a Child Health Web Portal for the prestigious Great Ormond Street Children’s Hospital NHS Trust (GOSH)/Institute of Child Health (ICH) based in London, UK.
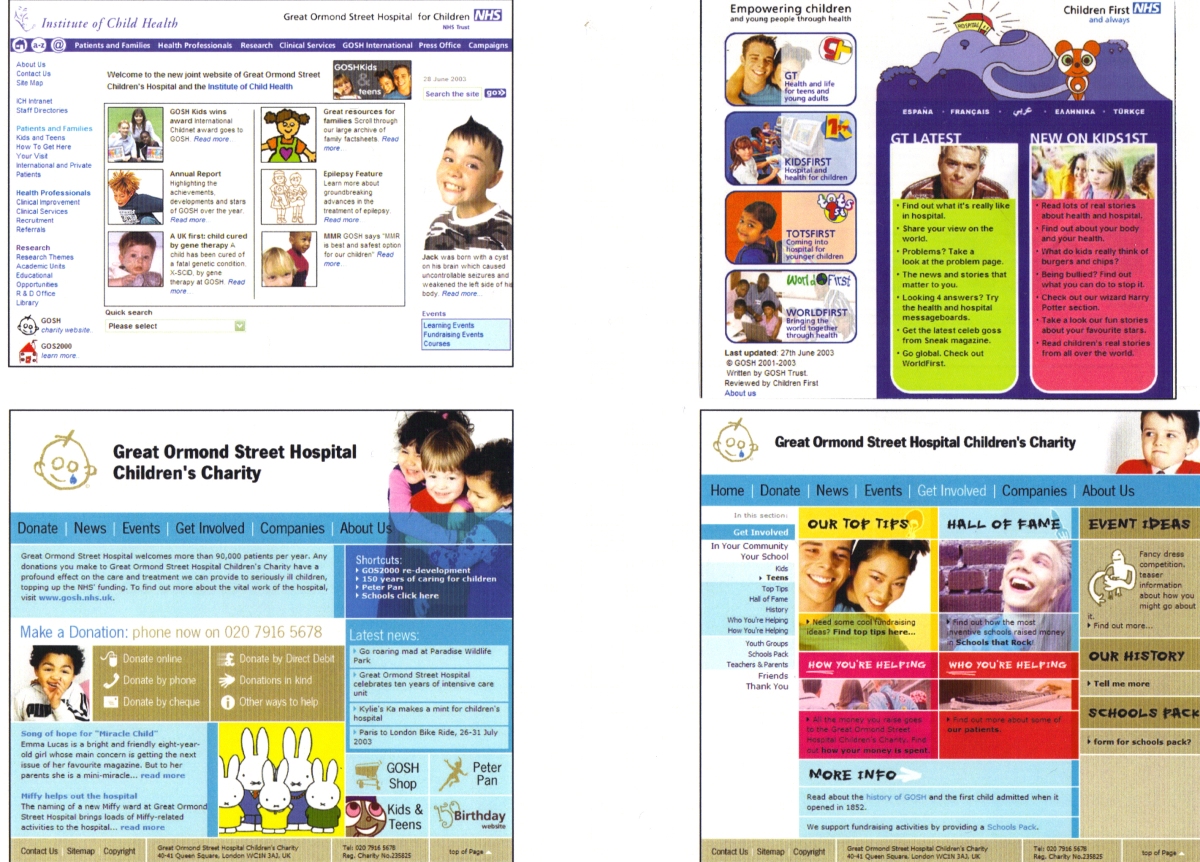
The project was intended to lead on innovation at the institutions and in the wider National Health Service (NHS) and was delivered in three phases. Screen grabs can be viewed below:
About
From the start, the project begged the question: Could we take a complex (and complicated) mandate and successfully achieve it in just two years? All under great public and media scrutiny (London being a world centre for media)? And how do you innovate for the 21st century in a major health care institution and build on its already high reputation?
Britain’s best-loved children’s hospital and charity, Great Ormond Street Hospital for Children NHS Trust (GOSH), contracted me to lead a two-year project to modernise the hospital’s web presence and take its brand into the 21st century. GOSH is both Britain’s first children’s hospital and a pioneering child health institution (along with its partner the Institute for Child Health). The hospital’s outstanding reputation meant the project was carried out under intense public, media and professional scrutiny, and required a keen awareness of new media developments and the needs of the hospital’s patients, their families and the public. It drew on an extensive public consultation and the NHS Modernisation Plan and the Information for Health strategy – which had identified strong demand for services and information to be made available online – to develop this innovative online offering. The NHS had also set the goal of having 25 per cent of all its services accessible via the web.
From the start, the project represented a new phase in how the institutions communicated. An announcement in PR Week in April 2001 acknowledged this, declaring the role will deal “with what is increasingly becoming an important part of the press office and the hospital”. Prior to beginning the two-year project in 2001, the existing website was an amateurish affair and not suitable for an internationally renowned centre for paediatric treatment, training and research.
The UK had become out of step with wider web developments at that time and had to do a lot of catching up. But there was a ready audience for better web content already established in the country. By 2001, data showed 3 million children in the UK were using the Internet and 33 million UK citizens could access it through work, school or home.
By 2001, the Internet offered an estimated 100,000 health-related websites (most based in the United States, leaving a gap for high-quality information based on UK research and experience). Trust was key and this was a crucial part of the content strategy that was developed.
As lead staff member for the website, I was in charge of recruiting and managing staff and suppliers, liaising with stakeholders inside and outside the organisations, planning work and seeking opportunities and partnerships.
The project was developed in three, distinct phases. Screen grabs from these phases are available for download and evaluation. They also include web traffic statistics. This unique snapshot of a complex project as it unfolded, should prove useful for other e-health practitioners.
As an innovator, the project became a catalyst for numerous online and offline initiatives across the institutions. The website made enormous strides, winning a number of national and international awards and leapfrogging to become one of the best NHS-linked sites in the UK. Areas radically improved included the design and navigation, patient information for families, press office, and the development and launch of the award-winning children’s website.
Each stage was transparently communicated and accompanied by high-profile publicity campaigns: a necessity because the hospital relies heavily on public trust and funding to function.
The first phase involved getting buy-in on a new design vision, assembling a team, extensive work on migrating the very large legacy website into the new template, and exciting colleagues on the potential of the new child health portal vision. It was launched in September 2001.
Ask Dr Jane Collins, a regular column written by the Chief Executive Dr. Jane Collins for The Times newspaper, was one of the more popular features of the child health portal. The portal was also directly connected to the NHS Direct service with its extensive online health encyclopedia.
In 2001, the project launched an interactive Christmas child health advent calendar offering top tips from health professionals on how to have a safe holiday season. It showed what could be done with the improving web design and production skills of the team. The PDF can be viewed here: http://www.scribd.com/doc/44905926/Christmas-Advent-Calendar-for-GOSH-Child-Health-Portal-2001.
As another example, the hospital’s 150th birthday celebration on 14th February 2002, attended by Her Majesty the Queen (and celebrities, including Madonna), was accompanied by an online interactive history prepared by the project and was used to inform the wider public about the child health portal.
Phase two involved the launching of new content developed by some of the world’s top child health experts and scientists, substantial new resources for sick children and their families, an online awareness-raising campaign to drive traffic to the health portal as a trusted and reliable resource, plus a wider media campaign. Based on user experience testing and user feedback, changes were made to the design and content structure to make the portal more user-friendly and to follow best practice in web design at that time.
The overall child health portal also gave birth to a highly successful new resource, the award-winning Children First website in May 2002. This resource was a year in development and was calibrated by age to provide relevant resources to guide children through the hospital experience. It used high-quality animation and partnered with BBCi and BBC Science to create resources that would resonate with children and youth. It included high-profile elements such as the Write4GOSH children’s writing prize, attracting entries from around the world, with winners receiving prizes from Cherie Booth QC, Dannii Minogue and children’s writer Jacqueline Wilson.
Children First attracted an average of 700,000 visitors each month with over 800 children in its first year contributing to the site. It addressed a gap in the online marketplace for health resources written for children rather than for their parents and families. It also gave birth to its own project: The Virtual Children’s Hospital (VCH). Funded by the PPP Foundation in August 2002, it worked with a team of psychologists to meet the social, psychological and information needs of ill children.
In March 2003 the Commission for Health Improvement (CHI) in its review and assessment found, in answer to the question “What, if anything, did CHI find that the rest of the NHS can learn from?” at the hospital, it was the child health portal, because “The trust’s website has different sections for children and families as well as for health professionals. The website also has sections for children of different ages and a broad range of information leaflets is available to download. The website has 3.5 million hits per month.”
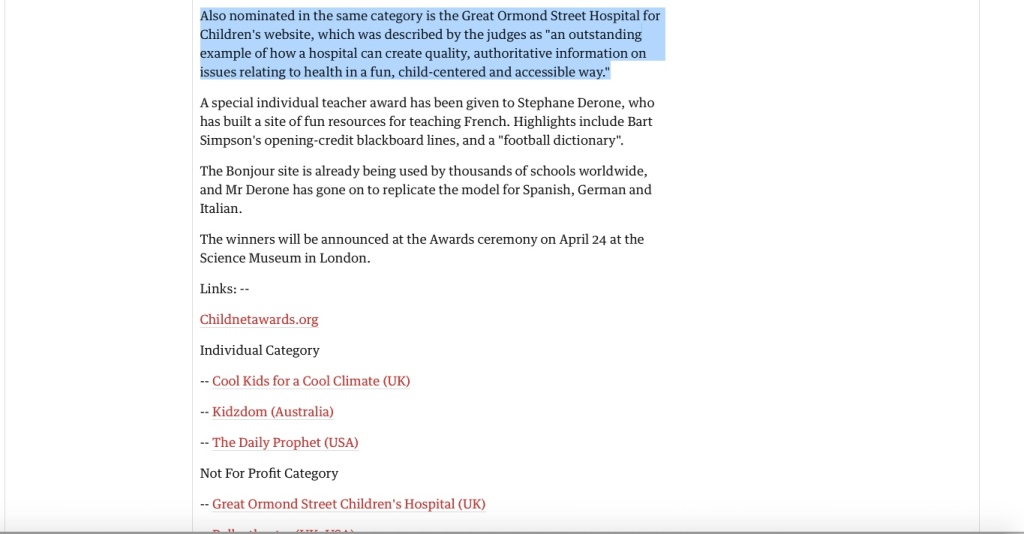
In 2003, the UK’s Guardian newspaper called the Children First website one of the “three most admired websites in the UK public and voluntary sectors,” and a UK government assessment called the overall GOSH child health web portal a role model for the NHS. Children First also won the prestigious Cable and Wireless Childnet Award that year as well. And was short-listed for the New Stateman’s New Media Awards.
In 2006, The Times of London called Children First the Top Child Health Website in its Wellbeing on the Web: The Best Portals survey (November 11, 2006).
Phase three saw online traffic growing at a steady clip, the portal gaining accolades, awards and positive reviews; it also helped the hospital to gain the highest rating in a government review (5*), and Children First was awarded significant further funding so it could expand its resources. The award-winning team also re-developed thewww.gosh.org charity website (one of the highest profile charity brands in the UK) and launched it in 2003 as well.
A great way to track the historical development of a web project is to use the Wayback Machine’s Internet archivehere (https://archive.org). By typing in the web address (for example, http://www.gosh.nhs.uk, and http://www.gosh.org), you can see a chronological history of the website by month.
Timeline
2001: Initial design vision articulated and team assembled. First phase of content creation and ‘soft launch’ of portal in September 2001. Begin experiments with new graphic design, including an online interactive Christmas advent calendar with health tips.
2002: Launch new content during the hospital’s 150th anniversary celebrations; begin development work on Children First content. Partnering with BBCi and BBC Science to improve quality of child and youth resources. Significant new content is launched throughout the year as the portal sees month-on-month growth in web traffic. Awarding of further funding for Children First and the Virtual Children’s Hospital.
2003: Winning of Childnet Award; launch of new GOSH Charity website. Record web traffic to the website.


Testimonials
“As a parent, I recognise how important it is to help your child understand all that they can about their stay in hospital and their care and treatment. Time spent in hospital can often be a very frightening experience. Making sure that your child has helpful, easy to read information will make a significant difference to their time in hospital.
I am sure that this website will prove very useful for children and their families.” Prime Minister Tony Blair, May 2002
“A highly attractive website written by and with children at Britain’s biggest specialist hospital for children. The site is carefully segmented for different age groups and provides a powerful platform on which children can reach out from the confines of their hospital wards, share their experiences and learn about a range of medical issues as well as have access to fun interactive resources.” Childnet Award 2003
“I am glad you mentioned the web site. If you can access it and haven’t recently please have a look. It has vastly improved and both David Latchman and I (it is a joint site with ICH) are very pleased.” Dr Jane Collins, Chief Exec’s Corner, Roundabout newsletter, February 2002
“I never thought that GOSHKids would be so valuable to the hospital or, more importantly, to children and young people attending the hospital or simply interested in health matters. I think that this reflects my age, though!
“Many of us over 30, even if we use the internet ourselves, are surprised how much children and young people use it both as a source of information and for entertainment.
“Even quite young children are using it routinely now and as an increasing number of families have access to it, either at home and/or at school or work, presumably more and more will do so.
“There are over 42,000 hits per day (1,260,000 a month) on our GOSHKids website already. Of course, part of the success of the website is down to its design and content. I would like to take this opportunity to congratulate Gary Loach, David South and the whole team who have worked so hard to make it successful.” Dr Jane Collins, Chief Exec’s Corner, Roundabout newsletter, June 2003
“The GOSH/ICH web site to date has been a notable success. Not only has it met a majority of its objectives as delineated in the PIN report of 2000 and achieved recognition as ‘exemplary’ among NHS resources, but it has also generated a number of spin-off projects, including Children First (as a successor to GOSHKids) and The Virtual Children’s Hospital.
“It has moved from providing a poor representation of the organisations, to above average for corporate web resources, and compares highly favourably with those of other NHS sites and departments. The most notable success lies in the resource it now provided for the public, especially GOSHKids.
“In a context in which less than 25% of all projects realise even 50% of their benefits, the satisfaction of 75% of the original objectives set out in the PIN report must rank as a significant achievement.” Website Project Audit by Passmasters Limited, 17 April 2003
“Great Ormond Street Hospital has launched this health site targeted specifically at childen, with a separate version aimed at young teenagers. The site aims to give young ‘uns information about health, illness and treatment in an easily digestable, non-threatening manner.” Internet Magazine, July 2002
“… it’s a good site and not just for those about to go into the hospital.” New Media Age, 20 June 2002
“The project was instrumental in pulling together a number of key strategies (including the NHS’s Modernisation Plan, and its Information for Health Strategy), and acting as a catalyst for numerous online and offline initiatives. Critical to these strategies is the need to provide information and services online and in an accessible way. The aim has not only been about serving the specific needs of the institutions, but also to become a broader child health portal.
“The website in 2001 was an amateurish affair and a disgrace to an internationally renowned centre for paediatric treatment, training and research. Run largely from the Research Office it was focused on one particular audience, uninspiring in design, reactive in updating and made little use of the potential of the internet. We needed someone to take it forward …
“David [South] was lead staff member for the website, recruiting and managing staff and suppliers, liaising with stakeholders inside and outside the organisations, planning work and seeking opportunities and partnerships. It is fair to say that the site made enormous strides under his leadership, winning a number of national and international awards, and leapfrogging to become one of the best NHS-linked sites in the UK.
“A number of areas were drastically improved, including design and navigation, patient information for families, press material, and the award-winning children’s site, which is now an international project with many different partners. David [South] project managed many projects in this time including linked sites for London IDEAS Genetics Knowledge Park, and the hospital charity site …” Stephen Cox, Chief Press Officer, Great Ormond Street Hospital for Children NHS Trust and the Institute of Child Health
Impact
Micro
- took public consultation and consultant’s report and crafted and developed a strategy to implement the GOSH Child Health Web Portal
- assembled team across two institutions
- set clear milestones and brought project management methodology previously deployed with the United Nations
- led on teaching new ways of project management for results
- took GOSH brand forward for the digital age
- advised colleagues on digital publishing and design
- awarded additional funding
Macro
- role model for NHS and government/charity sector. Awarded five stars in government review
- Childnet Award
- launched major milestones with well-known figures, including Her Majesty the Queen, Madonna, and pop stars
- significant media coverage of project
- attracted funding not only for the GOSH Child Health Portal but also for other projects at the institutions
- grew web traffic month-on-month, becoming one of the top online child health resources
- website cited in many other resources. One of the goals of the project was to increase access to high-quality child health resources and to have them cited in books etc.
Citations
The Great Ormond Street Hospital Manual of Children’s Nursing Practices by Susan Macqueen, Elizabeth Bruce and Faith Gibson, John Wiley & Sons, 2012
Help! My Child’s in Hospital by Becky Wauchope, Marbec Family Trust, 2012
Oxford Desk Reference: Nephrology by Jonathan Barratt, Peter Topham and Kevin P.G. Harris, Oxford University Press, 2008
Other Resources
GOSH Child Health Portal Phase 1a
GOSH Child Health Portal Phase 1b
GOSH Child Health Portal Phase 2a
GOSH Child Health Portal Phase 2b
GOSH Child Health Portal Phase 3
GOSH Project Launch Brochure and Screen Grabs, 2001-2003
GOSH Child Health Portal 2001 to 2003 Resources
Further Reading:
Embedding Young People’s Participation in Health Services: New Approaches edited by Louca-Mai Brady, Policy Press, 7 October 2020
“There is increasing interest in young people’s participation in the design and delivery of health services. But young people’s views are not consistently sought or acknowledged, and they are still often marginalised in healthcare encounters. Drawing on original research and a diverse range of practice examples, Brady explores the potential for inclusive and diverse approaches to young people’s participation in health services from the perspectives of young people, health professionals and other practitioners. She presents a practical new framework, embedded in children’s rights, that shows how young people’s participation can be integrated into services in ways that are meaningful, effective and sustainable.”

ORCID iD: https://orcid.org/0000-0001-5311-1052.
© David South Consulting 2024











You must be logged in to post a comment.